Rationale For Dental Implants
Dental implants do more than simply fill the gap of a missing tooth; by mimicking the lost root, they transmit chewing forces back to the bone and slow bone resorption. They replace the missing tooth independently without reducing adjacent teeth, preserving healthy teeth while providing more stable chewing and clearer speech. Compared with removable dentures, retention and comfort increase, and smile aesthetics and self-confidence improve. In the long term, they are more predictable and often more cost-effective than frequently renewed bridges and dentures. When the risk–benefit balance is correctly assessed, they are a biologically respectful, patient-centred treatment option.
Rationale for Dental Implants
Dental implants have transformed the way we think about replacing missing teeth. Instead of simply restoring what is visible in the mouth, implants allow us to rebuild the lost root and reconnect the prosthesis to the bone. The rationale for dental implants is therefore not only aesthetic but also biological, functional, psychological and long-term in nature. Understanding why implants are used helps both clinicians and patients make more informed decisions about treatment.
From tooth loss to implant thinking
Tooth loss has always been a major oral health problem. Traditional solutions – removable dentures and fixed bridges – aimed to fill the gap and restore appearance. However, they could not prevent ongoing bone resorption, changes in facial profile or the gradual loss of chewing efficiency. The development of osseointegrated implants introduced a new concept: replacing the tooth root within the bone and allowing the body to accept this new “artificial root” as part of the skeleton. This biological union changed the objective of treatment from simply “filling the space” to truly reconstructing the lost tooth.
Biological rationale: preserving bone and oral structures
After a tooth is extracted, the surrounding alveolar bone begins to resorb. The body no longer “needs” this bone to support a tooth, so it remodels and shrinks over time. Removable dentures sit on the mucosa and do not prevent this resorption; in fact, they can accelerate it by transmitting pressure to the bone surface. Fixed bridges rely on neighbouring teeth and ignore the empty socket beneath.
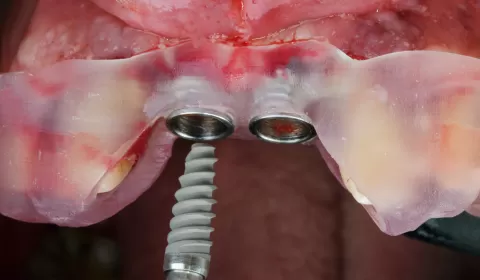
Dental implants provide a biological stimulus for bone maintenance. Through osseointegration – the direct contact between implant surface and bone – functional forces are transmitted through the implant into the surrounding bone. This loading helps preserve bone volume and shape, supports the soft tissues and contributes to a more stable facial profile, especially in the anterior maxilla where aesthetics are critical.
Functional rationale: restoring efficient chewing and speech
Chewing efficiency is strongly related to the stability and support of the prosthesis. Removable complete dentures often move during function, particularly in the lower jaw where the available surface is limited and the tongue competes for space. Many patients adapt by chewing slowly, avoiding certain foods or using only one side of the mouth. This can restrict nutrition and quality of life.
Implant-supported restorations are rigidly anchored to the bone, creating a stable platform for chewing. Patients report greater biting confidence, the ability to eat harder foods and a sensation closer to natural teeth. Speech can also improve, as the position and stability of the teeth are more precisely maintained. For partial edentulism, implants can replace single missing teeth without involving adjacent teeth, preserving natural proprioception and occlusal stability.
Prosthodontic rationale: protecting the remaining teeth
Conventional fixed bridges require tooth preparation of neighbouring teeth to create abutments. This often means removing healthy enamel and dentine from intact teeth, placing them under additional load and exposing them to future risk of caries, fracture or pulpal complications. In some cases, these abutment teeth eventually fail, expanding the edentulous span and complicating retreatment.
Dental implants allow single-tooth replacement without preparing adjacent teeth. The natural teeth remain untouched and continue to function independently. In longer spans or fully edentulous cases, implants can distribute occlusal forces more favourably than long-span bridges supported only by teeth. This protective effect on the remaining dentition is a key restorative rationale for choosing implants as part of a comprehensive treatment plan.
Aesthetic and psychosocial rationale
Tooth loss is not only a functional problem; it also has a strong emotional and social impact. Changes in smile line, lip support and facial proportions can alter self-image and social confidence. Removable dentures, especially if unstable, may cause embarrassment during eating, speaking or laughing. Some patients avoid social situations or adapt their behaviour to hide their prosthesis.
Implant-supported restorations can provide more natural aesthetics and better soft tissue support. The position of the crowns can be optimised without being constrained by clasps or denture flanges. Papillae and gingival contours can often be shaped around the implant crowns to mimic natural teeth, especially when treatment is carefully planned. Patients frequently report feeling that they “have their own teeth again,” which can positively affect self-esteem, social interactions and overall quality of life.
Long-term and economic rationale
At first glance, implant treatment may seem more expensive than conventional options. However, the rationale must also consider long-term value and life-span of the prosthesis. When a bridge fails due to decay or fracture of an abutment tooth, the repair often involves multiple teeth or complex retreatment, which increases both biological and financial cost. Removable dentures may need frequent relining or replacement as bone resorption continues.
Well-planned and well-maintained implants can achieve high long-term survival rates. By preserving bone and adjacent teeth, they may reduce the need for future extensive treatment. From a life-cycle perspective, implants can represent a cost-effective solution, particularly for younger patients who require restorations that will serve them for decades.
Rationale in different clinical scenarios
The reasons for choosing implants vary with the clinical situation:
-
In a single missing tooth, the main rationale is often to avoid preparing adjacent teeth while achieving ideal aesthetics and function.
-
In a posterior free-end saddle, implants can convert a removable partial denture into a fixed or more stable removable solution, greatly improving chewing and comfort.
-
In a completely edentulous mandible, even two implants supporting an overdenture can dramatically increase stability, making this indication one of the most compelling rationales in implant dentistry.
-
In the esthetic zone, implants enable emergence profile and soft tissue support that can be superior to removable options and many bridge designs, if bone and soft tissues are managed carefully.
Each scenario combines different elements of the general rationale: bone preservation, protection of remaining teeth, improved function and better quality of life.
Risk–benefit and medical rationale
No treatment is free of risk. The rationale for dental implants must therefore include a careful risk–benefit evaluation. Systemic conditions, medications, smoking, oral hygiene and patient expectations all influence the likelihood of success. For some patients, the surgical aspect or maintenance requirements may outweigh the expected benefits, leading the clinician to recommend alternative treatments.
However, for medically suitable patients who are motivated and able to maintain oral hygiene, the benefits of implants often clearly exceed the risks. Compared with repeated extractions, unstable dentures or heavily compromised bridges, implants can offer a more predictable and stable long-term outcome. The key is appropriate case selection, accurate diagnosis and comprehensive patient education.
Ethical and patient-centred rationale
Finally, the rationale for dental implants is also ethical. Modern dentistry aims to offer treatments that are conservative, biologically compatible and supportive of long-term oral health. By preserving bone and natural teeth, implants align well with these principles. At the same time, patient autonomy requires that individuals understand the options, costs, risks and expected outcomes before deciding.
Presenting implants as one option within a full spectrum of treatments – rather than as a universal solution – respects this ethical framework. The true rationale becomes collaborative: clinician and patient work together to select the approach that best matches medical conditions, anatomical possibilities, aesthetic goals and life circumstances.
Conclusion
Dental implants are not simply a fashionable technology or a luxury treatment. They are grounded in a strong biological, functional, prosthodontic and psychosocial rationale. By replacing the tooth root, preserving bone, protecting adjacent teeth and restoring stable function and aesthetics, implants address many of the limitations of traditional prostheses. When planned carefully and used in appropriate cases, they offer a long-term, patient-centred solution that fulfils the broader goals of contemporary dentistry: health, function and quality of life.

M. İhsan GÜRSOY / Diş Hekimi
Yazar