Why İs The Patient's Medical History Important İn Implants?
In dental implant surgery, a detailed medical history is fundamental to safe and predictable treatment. The patient's history of heart disease, diabetes, osteoporosis, autoimmune and neurological diseases, previous surgeries, allergies, and medications used determine the risks associated with bleeding, infection, and bone healing. Anticoagulants, bisphosphonates, corticosteroids, and chemotherapy drugs directly affect the surgical plan, type of anaesthesia, antibiotic requirements, and loading timing. Smoking, alcohol consumption, bruxism, poor oral hygiene, and a history of periodontal problems can reduce the long-term success of the implant. Age, mobility limitations, and cognitive status also alter prosthesis design and maintenance frequency. A regularly updated medical history provides a safer, patient-specific implant treatment. This reduces unnecessary risks, lowers the likelihood of emergencies, and protects both oral and general health in the long term.
Why is the Patient's Medical History Important in Dental Implants?
Dental implants are often described as a “routine” treatment, but there is nothing routine about placing a titanium screw into living bone. Behind every successful implant case stands a careful assessment of the patient’s overall health, medications and risk factors. A detailed medical history is not just paperwork; it is the safety net that protects the patient and helps the dentist plan predictable, long-lasting results.
Medical history as the first step in implant planning
Before scans, impressions or digital planning, a responsible clinician starts with one question: “Is this person medically suitable for implant surgery?” Medical history allows the team to see the patient as a whole, not just as a missing tooth. Information about heart disease, diabetes, bone problems, previous operations, allergies and current medicines shapes the entire treatment plan.
This background helps the dentist decide whether implants are appropriate at all, whether treatment should be done in the practice or a hospital setting, and whether adjustments are needed to the surgical technique, length of appointments, or type of anaesthesia. Without this information, even a technically perfect surgery may be unsafe.
General health and case selection
A thorough medical history helps classify patients according to how stable their general health is. Someone with well-controlled blood pressure and no major illnesses is very different from a patient with recent heart surgery, uncontrolled diabetes and severe breathing problems. Both may want implants, but they do not carry the same level of risk.
Certain conditions may require postponing implant surgery until a physician gives clearance. Recent heart attacks, strokes, severe lung disease, active infections or poorly controlled systemic illnesses can make implant surgery more dangerous. Knowing this in advance allows the dental team to coordinate with doctors, adjust or delay treatment and prevent medical emergencies in the chair.
Systemic diseases that affect healing and bone integration
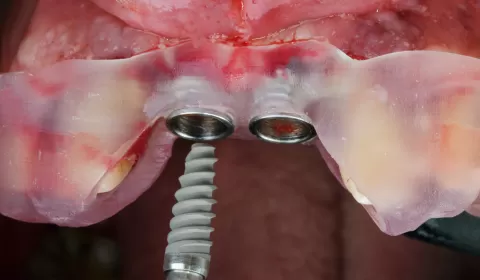
Dental implants rely on osseointegration – the direct, stable connection between bone and the implant surface. Many systemic diseases influence how well bone heals and how resistant tissues are to infection.
Well-known examples include diabetes, especially when poorly controlled, which can slow wound healing and increase the risk of infection. Cardiovascular disease may affect blood supply and tolerance for stress during surgery. Osteoporosis and other metabolic bone disorders can influence bone density and how firmly an implant can be anchored.
Autoimmune conditions and rheumatologic diseases, such as rheumatoid arthritis or scleroderma, may affect both healing and hand function, making oral hygiene more difficult. Neurological disorders like Parkinson’s disease can create tremor or reduced control, again influencing day-to-day cleaning around implants. A detailed history reveals these issues and allows for better planning, extra instruction and closer follow-up.
Medicines that change the way we plan surgery
A patient’s medication list is as important as their disease list. Many medicines directly affect bleeding, bone metabolism, immunity and the way the body responds to trauma.
• Anticoagulants and antiplatelet drugs (such as warfarin or certain heart medications) increase bleeding risk. Stopping them suddenly can be dangerous, but ignoring them can lead to excessive bleeding. The dentist uses the medical history to work with the physician to find a safe protocol.
• Bisphosphonates and other anti-resorptive drugs, often used for osteoporosis or cancer, are linked to medication-related osteonecrosis of the jaw. Identifying these patients before implant surgery is critical, because they may need modified treatment or sometimes complete avoidance of implants.
• Corticosteroids and immunosuppressive drugs reduce the body’s ability to fight infection and may impair healing.
• Diabetes medicines, chemotherapy agents, antidepressants and many other drugs can affect dry mouth, clotting, infection risk or bone quality.
Without a full medical history, the dental team cannot accurately weigh these factors. With it, they can adapt surgical timing, antibiotic choices, flap design and loading protocols to reduce complications.
Bleeding, infection and immune system risks
One of the key goals of reviewing medical history is to understand how the patient will respond to surgery. Conditions such as blood clotting disorders, anaemia or liver disease can increase the risk of bleeding or poor oxygen delivery to tissues. On the other side, immune problems, cancer therapies or poorly controlled diabetes may weaken the body’s defence against infection.
For some patients with specific heart problems or joint replacements, updated medical guidelines may recommend antibiotic prophylaxis under certain circumstances. Only by knowing the full medical picture can the dentist decide when additional protection is appropriate and when it is unnecessary.
This risk assessment helps determine whether implant surgery can be carried out safely under local anaesthesia in the clinic, whether sedation is appropriate, or whether closer monitoring in a hospital environment is safer.
Ageing, mobility and daily life factors
A patient’s medical history is not just a list of diseases; it is also a story about function and independence. Older patients may be living with arthritis, reduced vision, hand tremors or limited mobility. These factors directly affect how well they can clean around implants and prosthetic components.
A person may be medically stable but unable to manage complex hygiene routines. In such cases, the dentist might choose simpler prosthetic designs, larger hygiene access, or more frequent maintenance visits. The goal is not only to place implants successfully, but to ensure the patient can keep them healthy for many years.
Medical history also highlights conditions such as dementia, severe depression or other cognitive disorders. These can affect the patient’s ability to understand instructions, give informed consent and cooperate with long treatments. Recognising this early leads to more realistic expectations and often more conservative, supportive care plans.
Lifestyle, habits and dental history
Although often recorded separately, lifestyle and dental history sit naturally alongside medical history. Smoking, high alcohol intake, recreational drugs, bruxism and poor past dental compliance all influence implant prognosis. Smoking, for example, is strongly associated with higher implant failure and peri-implant disease rates, especially in combination with systemic illness.
Previous experiences with dentures, extractions, periodontal disease and failed restorations give important clues about the patient’s biology and behaviour. Frequent caries, aggressive periodontitis or a history of missed maintenance appointments alert the team that extra education, motivation and follow-up will be needed if implants are placed.
Medical history is also not a one-time form that lives forever in a folder. Patients develop new conditions, change medicines and experience life events between visits. Reviewing and updating the history before surgery, before restorative phases and during maintenance visits allows the team to spot new risks early – for example, the start of bisphosphonate therapy or a recent heart event – and adjust the implant plan before problems occur.
Designing safer, more predictable implant treatment
All of this information from the medical history feeds into one central aim: safe, predictable, personalised implant treatment. Rather than following a “one-size-fits-all” protocol, the clinician uses the patient’s individual risk profile to choose:
• Whether implants are appropriate at all
• How many implants to place and where
• The need for bone grafting or staged surgery
• The type of anaesthesia and length of appointments
• The timing of loading – immediate, early or delayed
• The maintenance schedule after restoration
By taking medical history seriously, the dental team is not trying to disqualify patients from treatment. Instead, they are protecting the patient’s general health while giving the implants the best chance to succeed.
In summary
A careful medical history is the foundation of responsible dental implant practice. It reveals hidden risks, guides communication with physicians, shapes the surgical plan and helps match the complexity of treatment to the patient’s real-world abilities. For the patient, it means fewer surprises, fewer complications and a treatment plan that respects both their mouth and their overall health. For the clinician, it turns implant placement from a mechanical procedure into a truly holistic, medically informed therapy.

M. İhsan GÜRSOY / Diş Hekimi
Yazar