Terminology In Implant Dentistry
Implant dentistry is a systematic field that relies on clear and consistent terminology. Accurate language standardises diagnosis, treatment planning, record keeping, scientific communication and teamwork. The core components are the implant, abutment and prosthesis; osseointegration describes the biological, stable union between implant and bone. Macro and micro implant design, connection types, platform shifting and loading protocols (immediate, early, delayed) guide clinical decisions. Single- or two-stage surgery, flap/flapless approaches and bone quality (D1–D4) determine the surgical strategy. Terms for peri-mucositis, peri-implantitis, mechanical complications and digital/guided surgery enable modern implantology to be performed safely, predictably and in a patient-centred way, while supporting clear patient communication and long-term maintenance.
Terminology in Implant Dentistry
Implant dentistry is a highly structured field, and its language reflects that structure. Clear terminology helps clinicians communicate with each other, with technicians and, most importantly, with patients. Understanding the basic and advanced terms is therefore not just academic; it shapes diagnosis, treatment planning and long-term maintenance. This chapter-style article reviews the core vocabulary of implant dentistry in a systematic and practical way.
Basic components: implant, abutment and prosthesis
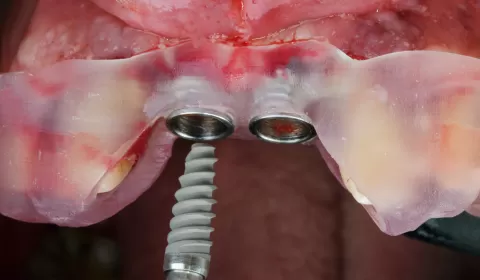
At the heart of implant dentistry are three main elements. The dental implant (often called the fixture or endosseous implant) is the part placed inside the bone. It functions as an artificial root and is usually made of titanium or a titanium alloy, although zirconia implants also exist.
On top of the implant sits the abutment. This is the connector that links the implant to the prosthesis. Abutments can be prefabricated, custom-milled, straight, angled, screw-retained or cement-retained. Each design affects emergence profile, soft tissue support and load direction.
Finally, the visible part is the prosthesis or implant-supported restoration. This can be a single crown, a bridge, an overdenture or a full-arch fixed restoration. When we say “implant crown”, we are referring to the prosthetic tooth that is attached to the implant via an abutment.
Osseointegration and bone–implant interface
A key term in implant dentistry is osseointegration. This describes the direct, stable contact between living bone and the implant surface at the microscopic level. There is no intervening fibrous tissue. This biological bond allows functional loading without pain or mobility.
The region where bone meets implant is the bone–implant interface. Concepts such as bone contact percentage, crestal bone level and marginal bone loss are used to evaluate how well this interface is maintained over time. These terms become central when discussing success criteria and long-term follow-up.
Implant design, macrostructure and microstructure
Implant bodies come in many shapes, and the wording reflects these differences. Cylindrical and tapered implants are common macro-designs. The external shape influences primary stability and how forces are distributed.
Most implants are threaded, meaning they have screw-like spirals along their surface. Terms such as pitch, depth and thread angle describe the geometry of these spirals. Thread design influences how the implant cuts into bone and how forces are transferred during function.
At the microscopic level, we talk about microstructure and surface topography. Implants can be machined, etched, sandblasted, coated or nanostructured. Descriptions like moderately rough or hydrophilic surface reflect how the surface has been treated to enhance osseointegration.
Connections: internal, external and platform concepts
The way the abutment connects to the implant is referred to as the implant–abutment connection. Classic designs include external hex, where the hexagon extends above the implant platform, and internal hex or internal conical connections, where the hex or cone is housed inside the implant body.
Two related terms are widely used in modern implant dentistry: platform matching and platform switching. Platform matching means the abutment diameter is the same as the implant platform. Platform switching means the abutment is narrower than the implant platform, creating a horizontal step. This concept has been linked to preservation of crestal bone and improved soft tissue stability.
Timing terminology: placement and loading
Several important terms relate to when the implant is placed and when it is loaded with a prosthesis. Immediate implant placement means the implant is inserted at the same appointment as tooth extraction, directly into the fresh socket. Early or delayed placement indicates that some healing time—weeks or months—has been allowed before drilling and implant insertion.
Similarly, immediate loading means a prosthesis is attached and the implant is put into function within a very short time, often within 48 hours of surgery. Early loading refers to loading after a few weeks, while conventional loading often means waiting around three months in the mandible and four to six months in the maxilla. The choice of timing is related to primary stability, bone quality and overall risk assessment.
Surgical concepts: one-stage, two-stage and flap approaches
The terms one-stage and two-stage surgery describe how implants are managed during healing. In a one-stage approach, the implant is placed and a healing abutment extends through the mucosa, so no second surgery is needed to uncover it. In a two-stage approach, the implant is completely covered by soft tissue during healing, and a second procedure later exposes it for abutment connection.
Another important set of words relates to flap design. A flapless procedure uses a punch or small incision without reflecting a full mucoperiosteal flap. A flap approach involves raising soft tissue to expose the bone. Terms such as crestal incision, vertical releasing incision, full-thickness flap and partial-thickness flap describe how the tissue is handled.
Bone quality, quantity and anatomical references
Implant planning frequently uses classifications of bone. The traditional Misch system describes bone density as D1, D2, D3 and D4. D1 is very dense cortical bone, while D4 is soft, fine trabecular bone. Terms like Type II bone or D3 bone quickly convey expected stability and drilling protocols.
Available bone refers to the height, width and length of bone in the proposed implant site. Words like crestal width, vertical deficiency, buccal undercut and sinus pneumatization indicate where limitations exist. Important anatomical structures are also codified: inferior alveolar nerve, mental foramen, maxillary sinus and incisive canal are key references during planning and surgery.
Prosthodontic terminology: retention, support and design
On the restorative side, we distinguish between screw-retained and cement-retained restorations. In screw-retained designs, an access hole allows the prosthesis to be removed via a screw. Cement-retained crowns are luted to the abutment, hiding hardware but introducing terms like residual cement and cement-induced peri-implantitis.
The way the prosthesis relates to soft tissues is also described. A hybrid prosthesis generally refers to a fixed full-arch restoration combining a metal framework with acrylic or composite teeth and pink material to replace missing gingiva. Overdentures are removable prostheses that gain retention from implants via locators, bars or ball attachments. Terms such as lip support, occlusal scheme, anterior guidance and posterior disclusion carry their usual prosthodontic meaning but are applied in the context of implants.
Complications and maintenance language
Modern implantology has its own vocabulary for complications. Peri-mucositis describes a reversible inflammatory lesion confined to the soft tissues around an implant, while peri-implantitis includes both soft tissue inflammation and progressive bone loss. Words like suppuration, pocket depth, bleeding on probing and bone defect morphology help define severity and guide treatment.
Implant failure can be early, when osseointegration was never achieved, or late, when a previously integrated implant loses stability. The broader term implant complication includes mechanical issues such as screw loosening, fracture, porcelain chipping and decementation of crowns. Maintenance protocols use terms like supportive peri-implant therapy, recall interval and risk-based maintenance schedule.
Digital and guided implant terminology
With the rise of digital dentistry, new terms have become standard. CBCT (cone beam computed tomography) and intraoral scanning provide data sets that are merged in implant planning software. Guided surgery uses a surgical template or guide fabricated from this virtual plan.
Within this workflow, phrases like prosthetically driven planning, virtual wax-up, sleeve-based systems and fully guided versus pilot-guided protocols describe how accurately the plan is transferred to the mouth. In the prosthetic phase, CAD/CAM abutments, monolithic zirconia and digital workflows signal an integrated digital approach from planning to delivery.
Why terminology matters
All of these terms are more than technical labels. They form a precise language that allows implant dentistry to be practised safely and predictably. When a clinician writes that a tapered, threaded, internal-connection implant was placed immediately after extraction in a one-stage approach and restored with a screw-retained crown under immediate loading, another clinician can picture the entire sequence. The terminology compresses complex biological and mechanical decisions into clear, shared words.
For students, mastering this vocabulary is the first step toward clinical competence. For experienced clinicians, careful use of terminology keeps records, research and communication accurate. And for patients, translated into everyday language, these terms help explain options, risks and expectations, turning a complex high-tech treatment into an understandable path back to function, aesthetics and oral health.

M. İhsan GÜRSOY / Diş Hekimi
Yazar