Short Dental Implants: When, How, and For Whom?
Short implants are a crucial alternative, especially for patients with limited vertical bone height, allowing them to achieve fixed teeth without bone augmentation. Thanks to modern systems, even internally connected screw-type implants as short as 4 mm can now be used safely. This makes it possible to avoid difficult and risky surgeries such as sinus lifts, vertical augmentation, or nerve lateralization in many cases.
What are short implants?
While implants shorter than 10 mm were once considered "short," current ITI and similar consensuses define 6 mm and shorter implants as "short implants." "Extra short" implants, such as 4 mm, have become an extremely valuable option in cases of limited bone height, thanks to appropriate materials and surface technology.
Due to modern alloys (e.g., high-strength titanium alloys) and hydrophilic, rough surfaces, the survival rates of short implants in properly selected cases have come very close to, and in some studies have even been found similar to, those of classic long implants.
Why are short implants preferred?
The most important advantage of short implants is that they reduce the need for bone augmentation. Especially in:
-
Upper jaw cases with chronic sinusitis, sinus pathologies, or contraindications for sinus lifts
-
Lower jaw distal regions with limited bone height just above the mandibular canal
-
Cases with significant vertical bone loss where the patient does not accept additional surgery, cost, or a long recovery period
short implants offer a less invasive, faster, and often more comfortable treatment option.
Who are short implants suitable for?
Although they seem attractive, short implants are not the right solution for "every patient." Common characteristics in suitable candidates include:
-
Limited but stable bone volume (especially cortical support)
-
Good oral hygiene and motivation for regular check-ups
-
Controlled systemic conditions (diabetes, osteoporosis, etc.)
-
If severe bruxism or parafunction exists, the occlusion must be manageable
If both the height and thickness of the bone are insufficient, if cortical support is weak, or if the patient generates high chewing forces when using the prosthesis, trying to solve the problem solely by "placing a short implant" can lead to long-term failure.
What does the scientific data say about short implants?
In older studies, the survival rates of short implants were lower than those of long implants. However, a significant portion of these studies involved:
-
The use of older generation smooth/machined-surface implants
-
Short implants being applied to more complicated, difficult cases
-
Surgical experience not always being sufficient
Clinical studies conducted after 2000 with systems featuring rough surfaces and advanced materials have shown that ≤ 6 mm short implants demonstrate similar survival rates to longer implants in appropriately selected cases. However, it is also emphasized that failure rates increase when used in D3–D4 type weak bone and with inexperienced surgical hands. In short, short implants are not "easy" but, on the contrary, are implants that "require experience."
Surgical Protocol: From Planning to Placement
The backbone of the short implant protocol is detailed planning:
-
Bone height, width, and adjacent anatomical structures (sinus, canal, mental foramen) must be clearly evaluated with CBCT.
-
In most cases, the under-preparation technique is used, drilling slightly narrower than the implant diameter to increase primary stability.
-
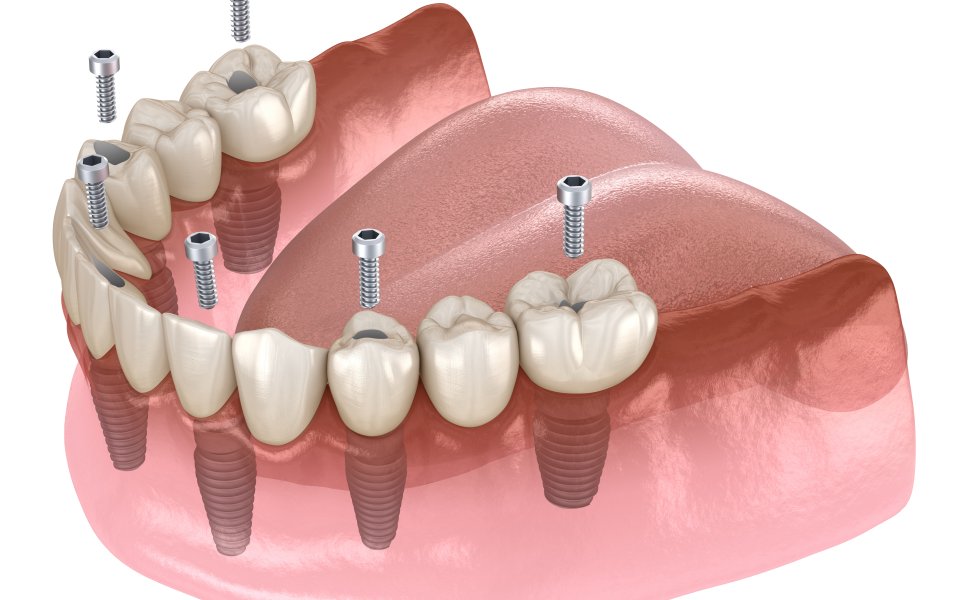
Since the surface area is limited in short implants, systems with wider diameters and aggressive macro-thread designs are preferred.
-
Torque values must be controlled; excessive torque in soft bone can lead to micro-fractures and late-stage bone loss.
Some 4–6 mm implant systems offer extra-short drills, taps, and kits with stoppers, making work, especially in the posterior region, practical and safe, while also significantly increasing patient comfort.
Placement Depth: Crestal, Subcrestal, or Transgingival?
In the classic approach, implants are usually placed subcrestally; because physiological bone loss of about 0.8–1.2 mm is expected within the first year. In short implants, this can affect a significant portion of the effective length. Therefore, some short implant designs are manufactured to be suitable for transgingival / equicrestal placement.
In these types of one-stage implants:
-
The marginal part of the implant has a form similar to a healing abutment.
-
Stability can be achieved even at 4–5 mm depth without excessive countersinking in the cortical bone.
-
Studies show that marginal bone loss is minimal in properly designed transgingival short implants.
However, working with this design requires greater surgical experience and precision than classic two-stage implants.
Prosthetic Protocols: Intelligent Management of Load
The long-term health of short implants largely depends on prosthetic planning. The basic principle is to increase axial loads and reduce lateral and bending forces:
-
Whenever possible, crowns on short implants should be splinted together.
-
Long cantilevered restorations on a single short implant should be avoided.
-
The occlusal table can be narrowed, and high-load areas like cusps and contacts should be adjusted in a controlled manner.
-
Contacts on the short implant during lateral movements (protrusive, laterotrusive) should be limited.
Temporary restorations should also be designed with a "controlled loading" logic; patients should be given clear instructions, especially within the first 3 months, regarding hard foods and unilateral chewing.
Short Implant Length Gains Meaning with a Smart Protocol
Short implants with a length of 4–6 mm, combined with modern material and surface technology, have become a strong and safe alternative in many cases where bone augmentation is undesired or not possible. However, success depends not on the length of the implant, but on:
-
Correct case selection
-
Detailed digital planning (CBCT, occlusion analysis)
-
Experienced surgical application
-
Prosthetic design with correctly engineered biomechanics
-
Regular maintenance and patient cooperation
In short, when used with the correct protocol, short implants can be as predictable as long implants; when used with the wrong protocol, their speed of causing problems can also be "short." Therefore, the question for every case is the same: "What is the smartest, most biological, and safest path here?"</
Features
- []
Comprehensive Dental Treatment
From routine checkups to advanced treatments, we offer a complete range of treatments to protect and beautify your health. Our personalized approach ensures that your special needs are carefully met.
All Treatments
- What Is A Dental Implant? Who Is It For And How Long Does It Take?
- Immedıate Implant Treatment In 1 Day
- All On Sıx Dental Implant Treatment
- What İs A Single Tooth İmplant?
- All-on-four Implant Treatment
- Implant Treatment Under General Anesthesıa
- Implant-supported Brıdge Treatment
- Why Do Dental Implants Faıl? Perı-ımplantıtıs Treatment
- Implant Placement Wıth Bone Graft
- Short Implants
- Guided Implant Surgery Treatment
- Sinus Lift Treatment
- Custom Subperıosteal Implant Treatment
- Implant Placement Wıth Ilıac Graft
- Zygomatic Implant Treatment