What İs A Single Tooth İmplant ? A Natural-Looking and Permanent Solution
The absence of a single tooth affects not only aesthetics but also chewing efficiency, speech, and, over time, the position of neighboring teeth. A single tooth implant mimics the missing tooth, complete with its root, providing a natural-looking and long-lasting solution.
What is a single tooth implant?
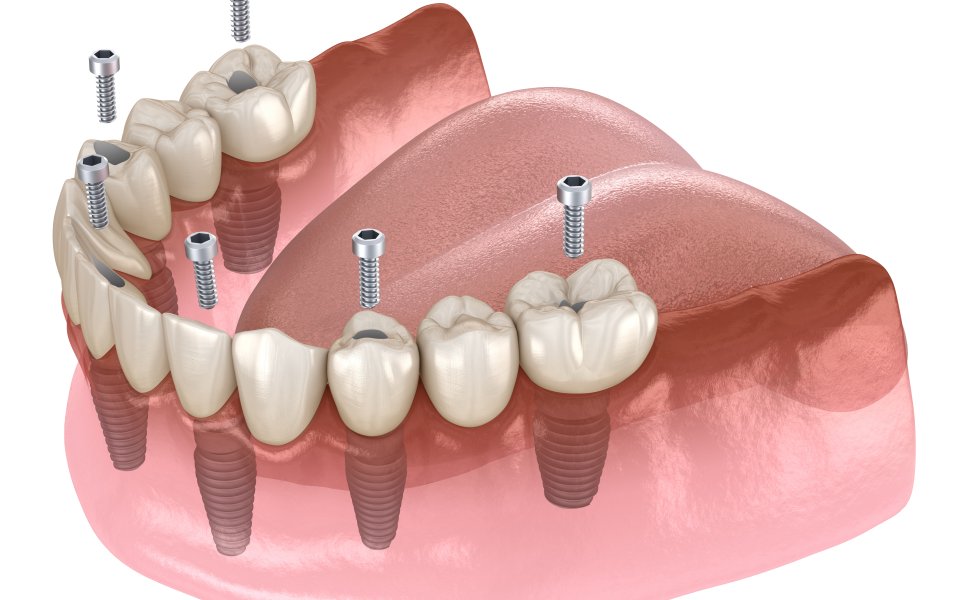
A single tooth implant is a fixed, lifelike replacement for one missing tooth. It consists of a small titanium or zirconia post placed in the jawbone, an abutment that connects above the gum, and a custom crown shaped and shaded to match the neighbors. After placement, the implant bonds with bone (osseointegration), creating a stable foundation that functions like a natural root.
Compared with a traditional bridge, a single implant preserves enamel because adjacent teeth do not need to be ground down for crowns. It also helps maintain bone volume in the missing area, supports healthy gum contours, and makes flossing easier because it is cleaned like an individual tooth rather than a multi-unit restoration.
The process typically includes consultation and 3D imaging, implant placement under local anesthesia, a healing period of several weeks to months, and then attachment of the final crown. Many cases allow a temporary tooth on the same day. Most patients report minimal discomfort managed with routine analgesics.
Good candidates have adequate bone and healthy gums; smokers or patients with uncontrolled diabetes may need additional planning. With regular hygiene and checkups, single tooth implants show high long-term success and feel natural when chewing and smiling.
Who is a single tooth implant suitable for?
A single tooth implant suits adults who are missing one tooth and want a fixed, natural-looking replacement without touching neighboring teeth. Ideal candidates have good general health, healthy gums, and enough bone volume at the site; this is confirmed with clinical exam and 3D imaging. Implants are especially appropriate when adjacent teeth are intact (avoiding a bridge) or when a removable partial is undesirable.
Patients who grind their teeth can still be candidates with protective nightguards. Smokers, and those with uncontrolled diabetes or active periodontal disease, may need stabilization or risk reduction before treatment. After growth is complete, many young adults missing a lateral incisor congenitally also benefit.
Requirements include excellent oral hygiene, willingness to attend follow-ups, and realistic expectations about healing time. With these conditions met, a single implant offers long-term function, preserves bone and gum contours, and is maintained like a natural tooth with routine brushing, flossing, and professional care.
How is single tooth implant treatment planned?
Planning starts with diagnosis: medical/dental history, periodontal exam, and photos. A CBCT scan and intraoral/digital impressions map bone volume, nerve/sinus position, and soft-tissue contours. Using this data, the clinician virtually positions the implant for ideal prosthetic emergence, selects diameter/length, and designs a surgical guide if needed. If bone or soft tissue is insufficient, grafting or contour augmentation is planned first. On surgery day, atraumatic placement targets primary stability; a temporary crown may be fitted immediately when conditions allow. After 8–12 weeks of healing, the final abutment and custom crown are delivered, occlusion is fine-tuned, and a maintenance plan (hygiene, nightguard if bruxism) is set.
Single tooth implant step by step process
Here’s the single-tooth implant journey, step by step:
-
Assessment
Medical/dental history, periodontal exam, bite analysis, photos. -
3D records
CBCT for bone and anatomy; intraoral/digital scan for teeth and soft tissue. -
Prosthetic-driven plan
Virtual implant position, diameter/length, emergence profile; decide on screw- vs cement-retained; fabricate a surgical guide if needed. -
Site optimization (if required)
Socket preservation, ridge augmentation, sinus lift, or soft-tissue grafting. -
Surgery day
Local anesthesia; flapless or minimally invasive access; osteotomy preparation; implant placement with primary stability (record torque/ISQ). -
Immediate decision
If stability and occlusion allow: place a healing abutment or non-functional provisional. Otherwise: cover screw + sutures. -
Post-op care
Analgesics, chlorhexidine rinse, soft diet, limited brushing at site; review in 7–10 days. -
Osseointegration
Typical timelines: mandible ~6–12 weeks, maxilla ~8–16+ weeks (patient factors may extend). -
Tissue shaping
Provisional or customized healing abutment to sculpt papillae and emergence profile. -
Final impressions/scans
Scan body or impression coping; shade match and material selection (zirconia, lithium disilicate over Ti-base, etc.). -
Delivery
Seat abutment and crown; torque to spec; verify passive fit, contacts, occlusion; baseline periapical radiograph. -
Maintenance
Daily brushing + interdental cleaning, 3–6 month recalls, peri-implant probing/radiographs as indicated; nightguard for bruxers; risk review (smoking, diabetesComparison of dental bridges and single-tooth implants
Comparison of dental bridges and single-tooth implants
Both options replace a missing tooth, but they differ biologically and practically. A dental bridge joins a false tooth to crowns on the neighbors; it’s faster and may cost less upfront, yet requires grinding healthy enamel and does not preserve the underlying bone. Hygiene is trickier because floss must pass under the pontic, and failures often involve decay or endodontic problems on the abutments. A single-tooth implant places a titanium or zirconia root in the bone, leaving adjacent teeth untouched. It helps maintain bone and gum contours, is cleaned like a natural tooth, and offers longevity when risks are controlled.
Possible risks and factors affecting success
Here’s the short, clinically honest version for single-tooth implants.
Possible risks
-
Surgical: pain/swelling, infection, bleeding, nerve or sinus involvement, implant malposition, early loss of primary stability.
-
Biologic (after healing): mucositis → peri-implantitis, progressive bone loss, soft-tissue recession, papilla loss/black triangles, hypersensitivity to cements.
-
Mechanical: screw loosening, abutment/crown fracture, ceramic chipping, implant fracture (rare), abutment or interface wear.
-
Aesthetic/functional: unfavorable emergence profile, mid-facial recession in thin biotypes, phonetic issues, occlusal overload.
Factors affecting success
-
Patient: smoking, uncontrolled diabetes, poor oral hygiene, active periodontitis, bruxism (unprotected), inadequate keratinized tissue, thin biotype.
-
Site: insufficient bone volume/density, dehiscence/fenestration, unfavorable ridge anatomy, proximity to adjacent roots.
-
Planning: prosthetic-driven positioning, 3D imaging, need for GBR/sinus lift/soft-tissue grafts, correct implant diameter/length.
-
Surgery: atraumatic technique, primary stability, contamination control, appropriate insertion torque and irrigation.
-
Prosthetics: screw-retained where feasible, cleansable contours, proper occlusion (light contacts, no excursive overload), verified torque, high-quality materials.
-
Maintenance: patient compliance, tailored recall (3–6 ay), bruxism nightguard, risk factor control.
Recovery and care recommendations
Features
- []
Comprehensive Dental Treatment
From routine checkups to advanced treatments, we offer a complete range of treatments to protect and beautify your health. Our personalized approach ensures that your special needs are carefully met.
Areas We Serve
What İs A Single Tooth İmplant? – Areas We Serve
We deliver chairside implant and dental treatments across every district of Istanbul with local expert teams.
Sancaktepe Single Tooth Implant Treatment
Dental implants are artificial tooth roots that restore function and aesthetics. Made of tissue-friendly titanium, they fuse with the jawbone for a durable stru...
All Treatments
- What Is A Dental Implant? Who Is It For And How Long Does It Take?
- Immedıate Implant Treatment In 1 Day
- All On Sıx Dental Implant Treatment
- What İs A Single Tooth İmplant?
- All-on-four Implant Treatment
- Implant Treatment Under General Anesthesıa
- Implant-supported Brıdge Treatment
- Why Do Dental Implants Faıl? Perı-ımplantıtıs Treatment
- Implant Placement Wıth Bone Graft
- Short Implants
- Guided Implant Surgery Treatment
- Sinus Lift Treatment
- Custom Subperıosteal Implant Treatment
- Implant Placement Wıth Ilıac Graft
- Zygomatic Implant Treatment